Want to know more?
Benign Brain Tumours (non-cancerous)
Generally, low-grade brain tumours – grade 1 or 2 – are slow growing and unlikely to spread. They are usually benign (non-cancerous), which means they tend to stay in one place and do not invade other areas of the brain or spread to other parts of the body.
Sometimes, they can be surgically removed and will not come back, causing no further problems. But some grade 2 tumours may grow back.
Malignant Brain Tumours (cancerous)
Malignant brain tumours can be either primary or secondary. Most common malignant brain tumours are spread to the brain from tumours outside the brain (secondary tumours) and treatment aims to prolong life and relieve the symptoms.
Primary malignant tumours, or high-grade brain tumours (grade 3 or 4) which start in the brain, are generally fast-growing. These must be treated as soon as possible to prevent them from spreading to, and damaging, other parts of the brain and spinal cord.
Brain tumour symptoms & signs:
There are a number of brain tumour symptoms and signs, depending on the type of brain tumour and its location. Some symptoms may be very severe or may not be apparent at all.
Symptoms are abnormal changes you have felt, and signs are what other people have observed about you, such as a weakness in an arm or leg, or having difficulties with speech.
If you are experiencing symptoms and signs that are concerning you, the first step would be to visit your GP to discuss these and they can advise further.
Brain tumour symptoms can include:
| Symptom | Comment |
| Headaches | Headaches which are more severe in the morning and wake you in the night. They are usually different from headaches you might have had previously and will be persistent and worsen with time |
| Nausea and vomiting | With a headache this can indicate increased pressure in the head (raised intracranial pressure). |
| Seizures | A seizure is abnormal electrical impulses in the brain, causing sudden involuntary changes in movement or function, sensation, awareness, or behaviour. A first time seizure in an adult is often investigated. |
| Weakness, loss of sensation or numbness | This is a sign of pressure on (or damage to) a specific part of the brain and can also be manifested through walking unsteadily or lack of coordination (ataxia) or muscle weakness on one side of the body (hemiparesis). |
| Hearing loss | Could be a sign of an acoustic neuroma if it occurs only on one side. |
| Loss/disturbance of vision, including double vision | In one or both eyes could be a symptom, if there is a tumour pressing on the optic nerve or there is one affecting the visual pathways or if there is raised intracranial pressure. |
| Speech difficulties | May also include the loss of ability to write, speak or understand words. A person may have difficulty getting the right words out (expressive dysphasia) or difficulty articulating them (dysarthia). |
| Other brain tumour symptoms | Lack of concentration, confusion, memory loss, disorientation, drowsiness, change in behaviour. |
How a diagnosis of a brain tumour is made:
You cannot see or feel a brain tumour during a routine examination. In order to determine whether you have a brain tumour, and to investigate the symptoms or signs you have presented with, you will be referred for a scan.
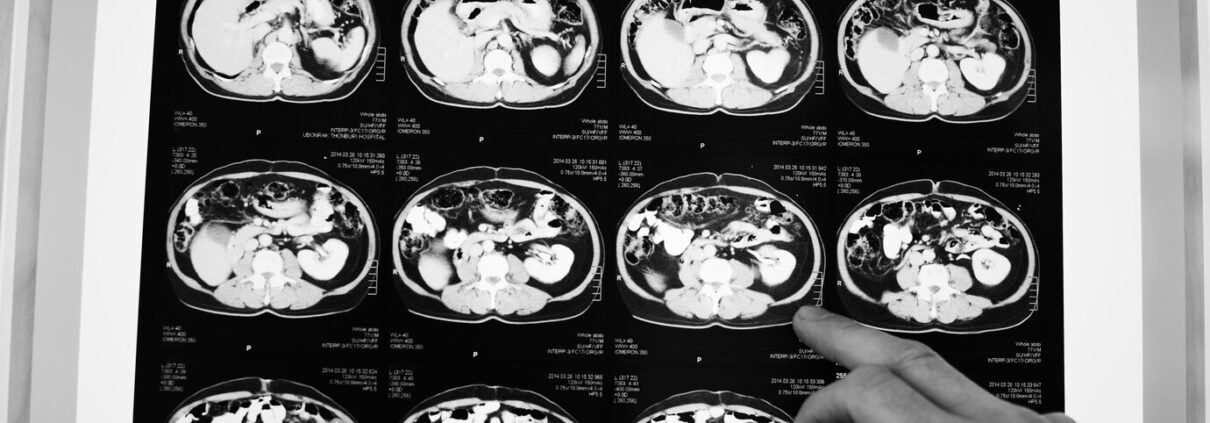
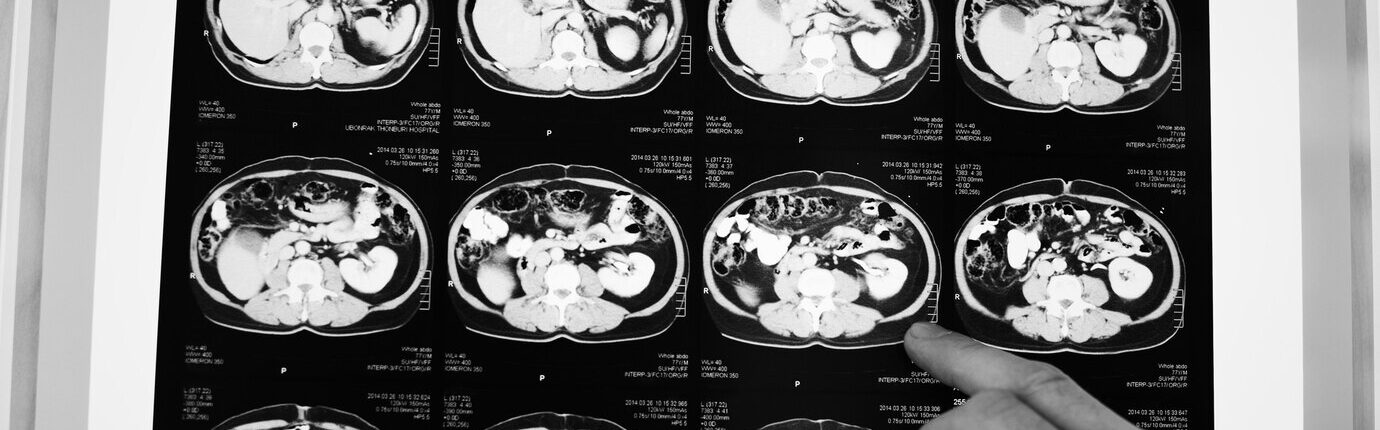
Brain tumours are identified using a CT or MRI scan. An expert who interprets scans (radiologist) will be able to see if you have an abnormality, which they may call a tumour.
If it is suspected that you have a brain tumour, your scans will be discussed at a neuroscience MDT (multidisciplinary team) meeting. MDT meetings are held weekly and you should receive the results of your scan around 5 days after the MDT meeting.
MRI and CT scans
Below you will find information about MRI and CT scans, how they work and the differences between them:
MRI scan
MRI stand for magnetic resonance imaging. This type of scan uses magnetic and radio waves, so no exposure to X-rays or any damaging forms of radiation. An MRI scan takes pictures from any direction. Contrast agents (usually gadolinium) can be used to delineate the lesion. These are usually injected into the arm during the scan. This has made some of our patients feel sick but this could be the thought of the injection. Needles are scary things.
Just a word about pacemakers; you may not be able to have an MRI scan if you have a pacemaker fitted or other metal objects in your body but alternatives are offered. Some new pacemakers are MRI compatible though – you will need to check with your cardiologist.
The scan will last about 45 minutes and can be noisy. Some hospitals let you listen to a CD so take one just in case.
Other tips – wear warm clothing; it can be chilly in the room. You will need to take off jewellery and anything else metal. This includes underwired bras and jeans with studs in.
If you have a child undergoing an MRI scan, get them to imagine they are going into a space capsule.
You should receive the results within two weeks. Privately, you can have the scan and reporting done on the same day, but private scans can be expensive. You can get one done privately with a report for a little over £200 – it depends where you go.
CT scan – computerised tomography.
Instead of sending out a single x-ray through the body, several beams are sent simultaneously from different angles. The computer then processes the results showing them as a 2D picture. CT scans are less expensive and take less time than an MRI scan, but they have lower resolution so could potentially not show some skull base and low grade tumours, as well as an MRI scan. So, if you have one type of scan rather than another, it is usually because one will be more suited to you.
A CT scan usually lasts around 20 minutes and is quieter than an MRI scan. You lie on a table and the scanner moves around your head. If you need a contrast scan, then an iodine-based contrast agent will be injected. This shows the ‘leaky’ blood vessels in a tumour and enables the neuroradiologist to see the mass directly.
Other tips – Warm clothing is recommended; it can be chilly in the room. And if you are allergic to shellfish let the radiographer know, because some contrast agents contain iodine.
Reporting is usually done within two weeks. Again – this may be sooner if you have a private CT scan.